Introduction
For many women, hair loss is a challenging and emotional experience. If you’re noticing a widening part or a general reduction in volume, you are not alone. Female pattern hair loss (FPHL) is the most common cause of hair thinning in women, and it’s a condition that can be effectively managed. This guide is designed to provide you with a clear, evidence-based roadmap to understanding your condition, exploring your options, and taking control.
Table of Contents
What is Female Pattern Hair Loss?
Female Pattern Hair Loss (FPHL) is the most common cause of hair loss in women. Unlike male pattern baldness, FPHL is a condition of diffuse hair thinning that can emerge at any age, although it becomes significantly more common after menopause. It’s a chronic and progressive condition, meaning it will likely worsen over time without intervention.
The Distinct Pattern of FPHL
Instead of a receding hairline or a bald patch, FPHL typically presents as:
- A widening of the central hair part, often described as a “Christmas tree pattern.”
- A diffuse reduction in overall hair density across the top of the scalp.
- A preserved frontal hairline.
A receding hairline or a completely bald area is rare unless a woman has abnormally high levels of male hormones (androgens).
The Lived Experience: More Than Just a Cosmetic Concern
The impact of FPHL goes far beyond its physical appearance. For many women, hair is central to their identity and self-image, and its loss can lead to:
- Emotional distress, anxiety, and depression.
- Profound feelings of isolation, shame, and a loss of confidence.
- A deep-seated sense of a loss of femininity and self-worth.
This psychological and emotional burden is a central part of the disease. A successful management plan for FPHL must not only address the physical symptoms but also provide support for this emotional toll, which is a crucial step toward holistic care and empowerment.
Causes of Female Hair Thinning
Key Hormones: Androgens vs. Oestrogens
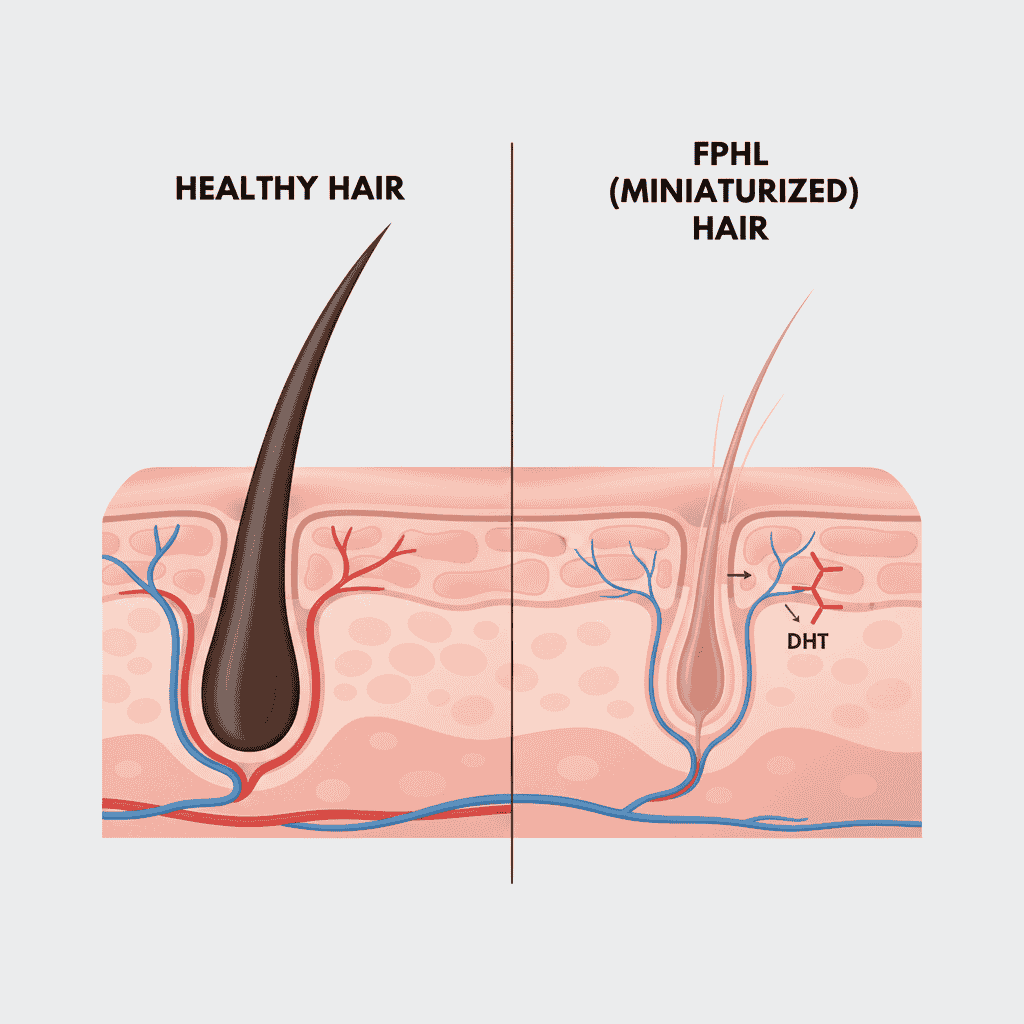
Dihydrotestosterone (DHT):
- The main hormone linked to FPHL.
- Even though women make much less DHT than men, it can still trigger follicle miniaturization (shrinking of hair follicles) in genetically predisposed women.
Oestrogens (female hormones):
- Help protect hair and prolong the growth phase.
- An enzyme called aromatase converts testosterone into oestrogen, offering some natural protection.
- When oestrogen levels fall (e.g., after menopause), the balance shifts in favour of androgens, often worsening hair loss.
Systemic Connections: A Window Into Overall Health
FPHL is not just a cosmetic issue — in some women, it may act as a warning sign for underlying health conditions:
Hormonal Disorders:
- Polycystic ovary syndrome (PCOS): Excess androgens can drive hair thinning.
- Adrenal hyperplasia or ovarian/adrenal tumours (rare): May present first with hair loss.
Metabolic & Cardiovascular Risks:
Studies show women with patterned hair loss may have higher chances of:
- High blood pressure (hypertension)
- Heart disease
- Type 2 diabetes and metabolic syndrome
While research shows strong associations, the exact cause-and-effect link is not fully proven.
Symptoms and Stages of Female Pattern Hair Loss
Female pattern hair loss (FPHL) develops gradually, often making it difficult to recognize in the early stages. Unlike sudden shedding conditions, it progresses in a slow but steady pattern.
Common Symptoms
- Hair feels less dense, especially along the crown and mid-scalp.
- Increased hair shedding noticed on pillows, in the shower, or during brushing.
- Miniaturized hairs appear: shorter, finer, and lighter in color compared to surrounding strands.
- The scalp may begin to show through under bright light or when the hair is parted.
Stages of Progression
- Early Stage: Subtle reduction in density, often noticed only in photographs or when styling hair.
- Moderate Stage: Thinning becomes more visible, with widening of the central part (“Christmas tree” appearance).
- Advanced Stage: Marked reduction in volume at the crown and top of the scalp, while the frontal hairline is usually preserved. In some women with higher androgen activity, temple thinning (bitemporal recession) may also develop.
Why Early Recognition Matters
Because hair follicles remain alive, timely intervention can preserve thickness, slow progression, and in some cases restore density. Delayed treatment often reduces the chance of meaningful regrowth.
The Diagnostic Journey: How Doctors Confirm FPHL
Getting the right diagnosis is the first step to treating female pattern hair loss (FPHL). Dermatologists use a mix of history, examination, simple in-clinic tests, and sometimes blood work to make sure the condition is correctly identified.
1. Talking to Your Doctor & First Examination
YOUR DOCTOR WILL ASK ABOUT:
- When you first noticed hair thinning, to determine whether hair loss is recent or gradual.
- Whether hair loss runs in the family, which may indicate genetic predisposition.
- Menstrual cycle details (irregular periods may hint at hormone imbalance such as PCOS).
They Will Examine Your Scalp To Look For
- Diffuse thinning (overall reduced hair density)
- Widening of the parting line (a key sign of FPHL)
- Other signs of high androgens, such as acne, excess body/facial hair, or irregular periods
Tip: Early detection can help preserve existing hair before significant thinning occurs.
2. Simple In-clinic Tests
Pull Test:
- The doctor gently tugs on a small bundle of hairs (10–20).
- If more than 2–3 hairs come out, it indicates active shedding.
Helps differentiate FPHL from normal hair fall or temporary shedding (telogen effluvium).
Wash Test:
- You collect hairs shed during washing over a few days.
- The doctor examines them to distinguish FPHL from other types of hair loss.
The presence of short, fine “vellus” hairs supports a diagnosis of FPHL.
Scalp Biopsy:
- Rarely needed, but a small tissue sample can be taken to confirm diagnosis or rule out inflammatory scalp disorders.
- Examining follicles under a microscope can show miniaturization, a hallmark of FPHL.
3. Essential Laboratory Investigations
Blood tests are not always required, but they help identify underlying causes or contributing factors.
Hormone Levels
- Free testosterone, DHEA-S, and prolactin to check for androgen excess.
- Abnormal results may indicate conditions like PCOS or adrenal disorders.
Nutrient Levels
- Iron and ferritin to detect deficiency, which can worsen hair thinning.
- Thyroid-stimulating hormone (TSH) to check for hypo- or hyperthyroidism.
- Vitamin D and other nutrients may also be checked to support overall hair health.
Tip: Lab tests help personalize treatment, ensuring therapies address both hair loss and any underlying medical conditions.
4. Clinical Patterns of FPHL
Dermatologists classify hair loss patterns to monitor progression and guide treatment. The main patterns include:
Diffuse Thinning with Preserved Frontal Hairline
- Hair becomes thinner across the top and crown, but the front hairline remains mostly intact.
- Follicles produce finer, shorter hairs.
- How the scale is used: Ludwig scale (3-point) and Sinclair scale (5-point) assign a grade to the thinning, helping doctors track progression over time.
- For example, Ludwig 1 = mild thinning, Ludwig 3 = severe thinning.
Thinning with Widening Central Part
- The part line on the scalp widens, forming a “Christmas tree” shape.
- Hair density decreases noticeably on either side of the part.
- How the scale is used: Olsen scale measures the width of the central part and surrounding thinning. It helps determine if treatment is needed and monitors response over time.
Thinning with Bitemporal Recession
- Hair thins at the temples, resembling male pattern hair loss.
- More common in women with high androgen levels.
- How the scale is used: Hamilton–Norwood scale assigns a stage based on the degree of recession, useful for tracking hair loss progression and comparing with baseline photos.
Tip: Knowing your hair loss pattern and scale stage allows your doctor to tailor treatments and monitor effectiveness accurately.
Treatment
Medications And Non-Surgical Treatments
Managing female pattern hair loss is about slowing down thinning, protecting existing hair, and encouraging regrowth. Since FPHL is a chronic and progressive condition, treatments usually need to be continued long-term to maintain results. If therapy is stopped, the benefits are gradually lost.
1. Topical Minoxidil (Rogaine)
Why it’s used: The only FDA-approved treatment for FPHL — it prolongs the growth phase and helps thicken thinning hairs.
- 2% solution: Twice daily; many women notice improvement within 6–8 months.
- 5% foam (off-label): Once daily; can be more effective for some but may increase scalp irritation or unwanted facial hair.
Note: A short-term increase in shedding (“dread shed”) is common and usually precedes new growth.
(see study: a comprehensive review on minoxidil for alopecia)
2. Oral Minoxidil (Low-Dose, Off-Label)
Overview: Originally a blood pressure medicine; low-dose versions are prescribed when topical minoxidil is ineffective or not tolerated.
Benefits & risks: Some women achieve better results with oral minoxidil, but it carries higher risk of systemic side effects such as excess body hair, swelling, or fast heartbeat.
(see review: Low-Dose Oral Minoxidil for Alopecia)
3. Antiandrogen Therapy
When it helps: Best for women with signs of high androgen activity (e.g., acne, PCOS).
Spironolactone: Can stop progression in many women and improve density in some cases. Requires blood pressure and electrolyte checks and may cause menstrual changes.
(see study: Spironolactone for Treatment of Female Pattern Hair Loss)
4. Finasteride & Dutasteride
How they work: Reduce DHT, the hormone that causes follicle shrinkage.
Notes: Used off-label in women. Low doses often don’t work for postmenopausal women, but higher doses or dutasteride may help. Important: Not safe during pregnancy due to risk of birth defects.
5. Hormonal Contraceptives
Who benefits: Women with hormone-related issues such as PCOS. Combination pills with low-androgen or antiandrogen progestins (like drospirenone) can help reduce androgen effects on hair follicles and are sometimes combined with other treatments.
Non-Pharmacological and Procedural Treatments
In addition to medications, several non-drug and procedural approaches can support hair regrowth or improve hair density in women with female pattern hair loss. These options range from innovative therapies like platelet-rich plasma to supportive lifestyle measures.
1. Platelet-Rich Plasma (PRP) Therapy
What it is: A small amount of the patient’s blood is drawn, processed to concentrate platelets, and then injected into the scalp.
How it works: Platelets contain growth factors that stimulate follicle stem cells, prolong the growth (anagen) phase, and improve blood supply to the scalp.
Evidence: Studies show PRP can significantly increase hair density and thickness. It is generally safe and well-tolerated, and often works best when combined with other treatments such as minoxidil or microneedling.
2. Low-Level Laser Therapy (LLLT)
Overview: FDA-cleared devices that use red light diodes to stimulate scalp circulation and boost follicle activity.
Evidence: A large controlled study found that LLLT significantly increased hair counts in both men and women after 26 weeks of use.
Pros: Safe, painless, non-invasive, and without reported side effects. More long-term studies are still needed to confirm results.
3. Surgical Hair Transplantation
What it is: Hair follicles are moved from dense “donor” areas (usually the back of the head) to thinning regions.
Limitations for women: Because female pattern hair loss often causes diffuse thinning across the entire scalp, donor areas may also be weak. This makes transplantation less effective or unsuitable for most women. It is usually considered only for women with stable hair loss and a strong donor area.
Success rate: In suitable candidates, hair transplants have success rates above 97%.
Stress Management
Chronic stress can worsen hair loss and trigger temporary shedding conditions like telogen effluvium. Stress-management practices such as mindfulness, yoga, breathing exercises, and adequate sleep can be valuable alongside medical treatments.
Nutritional & Lifestyle Support for FPHL
A balanced diet is essential for healthy hair growth. Research suggests that a Mediterranean-style diet — rich in raw vegetables, fresh herbs, whole grains, and healthy fats — may reduce the risk of androgenic alopecia.
Key Nutrients for Hair Health:
Protein – The building block of keratin (the main hair protein).
- Sources: Eggs, lean meats, fish, legumes, nuts, low-fat dairy.
Iron – Supports oxygen delivery to hair follicles. Deficiency is a common cause of hair loss in women.
- Sources: Spinach, lentils, red meat.
Vitamins A, B, C, D – Essential for cell turnover and follicle function.
Sources:
- A: Sweet potatoes, spinach
- B: Bananas, potatoes, whole grains
- C: Citrus fruits, leafy greens
- D: Sunlight, fortified foods, fatty fish
Zinc – Supports hair follicle repair and development.
- Sources: Nuts, seeds, whole grains.
Omega-3 Fatty Acids – Improve scalp and hair follicle health.
- Sources: Fatty fish (salmon, tuna), flaxseeds, walnuts, soybeans.
Camouflaging & Coping Strategies
The Emotional and Social Toll of FPHL
Psychological Burden
- Female pattern hair loss often lowers self-esteem and body image, with many women describing it as overwhelming and isolating. Feelings of anxiety, depression, and shame are common, especially due to societal pressure on women to have thick, healthy hair.

Social and Professional Challenges
- Hair loss can lead to withdrawal from social and romantic relationships. Surveys show many women experience marital strain and career setbacks. Stress worsens the cycle, as anxiety can trigger more shedding. Counseling and stress management are vital for breaking this loop.
Prognosis and Outlook
Progressive Nature
- Without treatment, FPHL usually worsens gradually, with unpredictable periods of shedding.
Hope with Early Care
- Since hair follicles remain alive, early treatment can slow, stop, or even reverse loss. Consistent, long-term management often restores not just hair, but also confidence and control.
Prevention & Myths
Common Myths About Hair Loss
Misconceptions about hair loss can create unnecessary anxiety. Some common myths include
Hair loss only comes from the mother’s side.
- Genetics can be inherited from either parent; family history is important but not the sole determinant.
Wearing hats or styling hair causes baldness.
- Hair loss is not caused by hats, haircuts, or shampooing. Follicle miniaturization is internal, not due to external pressure.
Brushing frequently makes hair thicker.
- Over-brushing can actually damage hair and increase breakage. Gentle care is key.
Hair loss is purely cosmetic and harmless.
- FPHL may indicate hormonal imbalances or systemic conditions like PCOS, thyroid disorders, or nutrient deficiencies. Early evaluation is important.
Tip: Awareness and evidence-based care are more effective than following myths or unverified remedies.
FAQs
Can I use minoxidil while pregnant or breastfeeding?
It is not safe to use minoxidil during pregnancy or while breastfeeding. Although the risk is considered low, minoxidil can be absorbed into the bloodstream and may pose a risk to the developing fetus or baby. It’s crucial to stop all treatments and consult with your doctor if you are pregnant, planning to become pregnant, or breastfeeding.
What is the difference between FPHL and temporary hair shedding (telogen effluvium)?
FPHL is a chronic condition characterized by progressive miniaturization of hair follicles, leading to gradual thinning over months or years. Telogen effluvium, on the other hand, is a temporary condition that causes sudden, widespread hair shedding, often triggered by a major stressful event like childbirth, surgery, or severe illness. While it can be alarming, telogen effluvium usually resolves on its own within a few months, whereas FPHL requires long-term treatment.
How does menopause affect female pattern hair loss?
Menopause can significantly accelerate the progression of FPHL. As estrogen levels decline, the relative effect of androgens on hair follicles can increase. This hormonal shift often leads to more rapid thinning in women who are genetically predisposed to the condition. This is why it’s common for FPHL to become much more noticeable around the time of menopause.
Are treatments for FPHL covered by insurance?
It depends on your insurance plan. Many treatments for FPHL are considered cosmetic and may not be covered. Prescription medications like oral minoxidil or spironolactone may be covered, especially if they are prescribed to treat an underlying condition like PCOS. Over-the-counter options like topical minoxidil are typically not covered. It’s best to check with your insurance provider to understand your specific benefits.
Can chronic stress cause FPHL?
While stress alone does not cause FPHL, it can absolutely make it worse. Chronic stress can trigger telogen effluvium, which can be a co-existing condition with FPHL. This can lead to a period of more intense hair shedding and make the underlying FPHL appear much more severe. Managing stress is an important part of a holistic treatment plan.
Conclusion
While FPHL is a complex condition, it is also a manageable one. This guide has provided you with the knowledge to understand its causes, recognize its symptoms, and explore a range of solutions. The key takeaway is simple: early diagnosis and consistent, long-term care are crucial. By taking a proactive approach and consulting with a dermatologist, you can effectively treat your hair loss and regain your confidence.