introduction
Have you ever noticed clumps of hair on your pillow, in the shower, or stuck to your hairbrush and felt that sudden wave of panic? You’re not alone. One of the most common reasons for sudden shedding is a condition called telogen effluvium (TE).
Table of Contents

What Is Telogen Effluvium (TE)? Understanding Temporary Hair Loss
Telogen Effluvium (TE) is a common form of non-scarring alopecia characterized by a significant and diffuse increase in hair shedding across the scalp. It is fundamentally a reactive process, meaning it is a direct biological response to a systemic disturbance or “shock” to the body, rather than a primary disease of the hair follicles.
One important thing to know: hair loss doesn’t happen immediately. The shedding usually appears 2–4 months after the triggering event, which is why many people are surprised when their hair starts falling out long after stress, illness, or other triggers.
- Core Definition: Excessive shedding of hair that has prematurely entered the resting (telogen) phase. The term “effluvium” literally means excessive shedding.
- Clinical Course: It can be acute (self-limiting) or chronic (prolonged course with insidious onset). While hair volume is significantly reduced, TE does not cause complete baldness.
The Biological Context: The Hair Growth Cycle
To understand TE, one must recognize the three normal phases of hair growth:

Anagen Phase (Growth):
The active and longest phase where hair follicles produce new hair shafts.
- Duration: Typically two to seven years.
- Normal Distribution: ≈85% to 90% of hair is in this phase.
Catagen Phase (Transition):
A brief, transitional stage where the follicle involutes and growth ceases.
- Duration: Only a few weeks (typically three to six).
Telogen Phase (Resting):
The hair enters a resting state as a “club hair” and remains dormant until shed.
- Duration: About three to five months.
- Normal Distribution: ≈10% to 15% of hair is in this phase.
Pathophysiology And Mechanism of Shedding
The central mechanism of Telogen Effluvium is the abrupt and premature signaling for a large, synchronous proportion of hair follicles to shift from the active Anagen Phase to the resting Telogen Phase.
The Mechanism and Time Delay
- The Shock: A metabolic or physiological “shock” to the body forces a large number of growing hairs to stop their growth early.
- The Lag Time: The key clinical feature is the physiological lag. The hair stops growing (enters telogen), but it remains anchored in the follicle for the full duration of the resting phase (averaging three months).
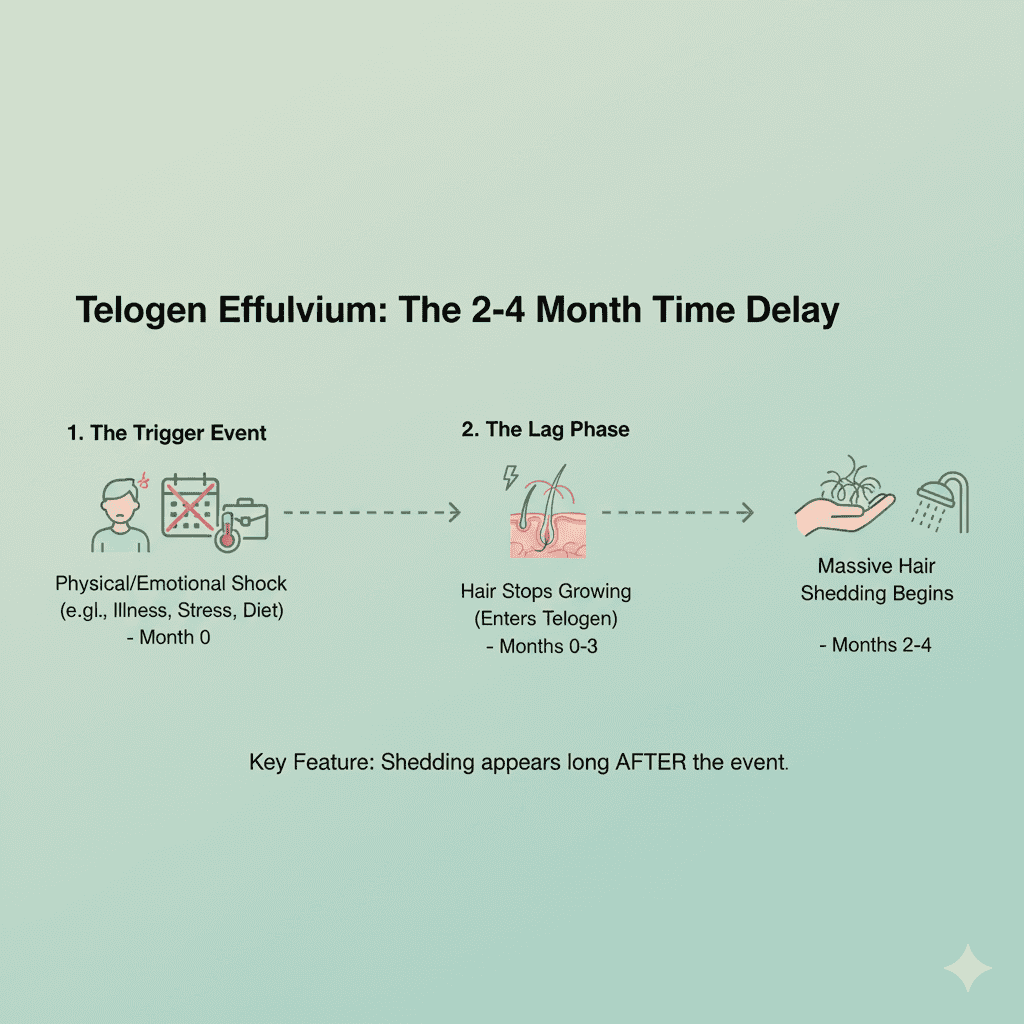
- The Shedding: Noticeable hair shedding only occurs two to four months after the initial trigger (e.g., a high fever or surgery) when a new anagen hair starts growing beneath it and physically pushes the old telogen hair out.
Deeper Mechanisms (Types of Disruption)
The specific way the cycle is disrupted can vary, leading to different clinical presentations:
- Immediate Anagen Release: The most common form, where a stressor causes a sudden, premature entry into telogen, leading to shedding ≈ two to three months later.
- Delayed Anagen Release: The anagen phase is prolonged, and the subsequent massive shift to telogen results in a heavy, but delayed, wave of shedding.
- Short Anagen Syndrome: Characterized by an idiopathic (unknown cause) shortening of the anagen phase, often associated with chronic TE and leading to persistent, fluctuating hair loss over time.
- Molecular Factors: The underlying cause disturbs the balance of growth factors, neuroendocrine signals, and cytokines that maintain follicle health, which ultimately accelerates the transition into the catagen phase.
Top Causes of Telogen Effluvium: Why Sudden Hair Shedding Happens
Telogen effluvium happens when the body goes through a shock or major change that disrupts the hair growth cycle. Here are the most common causes:
For more about what triggers TE, see Cleveland Clinic’s guide to Telogen Effluvium.
1. Physical & Emotional Stress
- illness & High Fever: Severe infections like COVID-19 or the flu can temporarily halt hair growth, causing many follicles to enter the resting phase at once.
- Major Surgery or Trauma: Physical stress or injury signals the body to prioritize vital organs over hair growth, triggering shedding.
- Crash Dieting / Rapid Weight Loss: Sudden nutrient deprivation, especially protein, reduces resources for hair production.
- Emotional Stress: Anxiety, grief, or major life changes can disturb hormonal balance and hair follicle cycling.
2. Hormonal & Endocrine Changes
- Postpartum Hair Loss: After childbirth, dropping estrogen levels signal many hairs to enter the telogen phase, causing shedding 2–5 months later.
- Thyroid Disorders: Both hypo- and hyperthyroidism disrupt the hair cycle, leading to diffuse shedding.
- Stopping Birth Control Pills: A sudden drop in estrogen can trigger temporary hair loss.
- Menopause: Hormonal fluctuations during menopause may increase shedding.
3. Medications (Drug-Induced TE)
Some medications interfere with the hair cycle, with shedding usually starting around 3 months after use.
- Blood pressure drugs (beta-blockers)
- Retinoids or too much vitamin A
- Blood thinners (heparin, warfarin)
- Antidepressants and anti-seizure drugs
- Chemotherapy drugs
- Weight-loss injections like Ozempic and Mounjaro
4. Nutritional Deficiencies
- Iron Deficiency: Low iron disrupts hair follicle metabolism, often causing shedding before anemia develops.
- Low Protein Intake: Hair is made of protein, so insufficient intake weakens growth.
- Zinc & Vitamins (B, C, D): These nutrients support follicle health and repair; deficiency can trigger TE.
5. Environmental & Lifestyle Triggers
- Toxins & Pollutants: Exposure to heavy metals or harmful chemicals may disturb the hair cycle.
- Severe Scalp Sunburn: Damage to follicles can temporarily increase shedding.
- Chronic Illness: Long-term conditions like autoimmune disease, kidney, or liver problems can stress the body.
- Poor Sleep & Fatigue: Consistently poor rest disrupts the body’s healing processes, including hair renewal.
Telogen Effluvium Symptoms: Diffuse Thinning Without Bald Patches
Telogen Effluvium (TE) doesn’t cause bald spots like alopecia areata or male pattern hair loss. Instead, the main sign is diffuse shedding—hair falling from all over the scalp. Here’s how it usually shows up:
The American Academy of Dermatology offers a helpful overview of different hair loss patterns and symptoms.
What You May Notice
- Sudden increase in hair fall: You may see extra hair on your pillow, in the shower drain, or stuck to your hairbrush.
- Overall thinning: Instead of patches, your hair looks less dense all over. Some people notice a wider parting or a thinner ponytail.
- Hair quality looks the same: The scalp is healthy, with no redness, itching, or scarring. The remaining hair is still normal.
- Scalp sensations (sometimes): A few people experience burning, tingling, or soreness on the scalp. This is called trichodynia.
Good to know: TE can be scary because of the amount of hair you see falling, but it never causes complete baldness.
Acute vs. Chronic TE – What’s the Difference?
- Acute TE: Starts suddenly, often 2–3 months after stress, illness, or surgery. You might shed 200–400 hairs a day, but the condition usually lasts less than 6 months. Most people see full recovery once the trigger is removed.
- Chronic TE: Lasts more than 6 months and often affects women in their 30s–50s. Shedding is moderate but ongoing (about 150–250 hairs a day). It can come and go for years, but it still doesn’t cause bald patches.
Key takeaway: If you notice more hair than usual falling out all over your scalp, especially after a stressful event or illness, it could be telogen effluvium. The good news is that in most cases, the hair grows back once the cause is managed.
How Doctors Diagnose Telogen Effluvium: Tests and Key Indicators
Telogen effluvium (TE) is diagnosed using a systematic approach that combines a detailed history, physical examination, and targeted lab tests. Here’s how doctors figure it out:
1. Patient History: Looking Back 2–3 Months
- Why it matters: Hair shedding usually shows up 2–3 months after the trigger, so doctors must ask about events that happened months earlier.
What they ask about:
- Severe illness or high fever
- Major surgery or trauma
- Emotional stress or major life changes
- New medications or stopping old ones (e.g., birth control pills, beta-blockers)
- Diet changes or rapid weight loss
2. Physical Examination: The Hair Pull Test (HPT)
Why it’s done:
To see if your hair is actively shedding more than normal.
How it works:
- The doctor gently grabs 40–60 hairs between their fingers.
- They pull gently along the hair shaft.
- Count how many hairs come out.
What the results mean:
- Normal: Less than 10% of hairs (usually 2–3 hairs) come out.
- Positive for (TE): More than 10% of hairs (4–6 or more) come out. Look for white bulbs at the roots—this shows the hair is in the resting (telogen) phase, which is typical in (TE).
Key Takeaway:Seeing white bulbs confirms that the shedding is from hairs in the resting phase, which is exactly what happens in telogen effluvium.
3. Laboratory Tests: Finding Hidden Causes
Why it’s done:
To check if anything in your body is triggering hair shedding and to rule out other causes.
Common tests include:
- Iron (Serum Ferritin): Measures iron levels, which are crucial for healthy hair growth. Low iron can make hair fall out faster.
- Thyroid Function Tests (TFTs): Checks if your thyroid is underactive or overactive, both of which can affect hair.
- Vitamin D: Optional, but low levels may affect hair health.
- Syphilis Test: Only needed if there are risk factors.
Key Takeaway:These tests help doctors figure out the underlying cause and guide the right treatment. For example, low iron may require supplements to help your hair grow back.
4. Scalp Biopsy: When to Consider It
When it’s needed:
If hair shedding continues for more than 6 months even after the trigger has been addressed
When it’s done:
- Makes sure the hair loss is really telogen effluvium (TE).
- Rules out other conditions that can look similar, like female pattern hair loss or chronic alopecia areata.
Bottom line:A scalp biopsy is usually a last step to double-check the diagnosis when hair loss doesn’t get better on its own.
5. Differential Diagnosis: TE vs. Female Pattern Hair Loss (FAGA)
Sometimes it’s hard to tell telogen effluvium (TE) apart from female androgenetic alopecia (FAGA) because both can cause diffuse hair thinning. Here’s how doctors distinguish them:
Hair Thickness:
- TE: Hair shafts are mostly uniform in thickness.
- FAGA: Hair shafts vary in size (miniaturization), with many thinner hairs.
Fine (Vellus) Hairs:
- TE: Few or none.
- FAGA: High number of fine, non-pigmented hairs.
Scalp Signs:
- TE: Minimal or no scalp changes.
- FAGA: May show pigmentation or yellow dots around follicles.
Pattern of Hair Loss:
- TE: Diffuses all over the scalp, no specific area.
- FAGA: Often starts in central or frontal areas.
Bottom Line:(TE) is usually temporary and self-limiting, while FAGA is progressive and needs early treatment to prevent permanent thinning.
6. Key Points for Patients
- TE is usually diagnosed based on symptoms—how your hair is shedding—supported by simple lab tests and the hair pull test.
- Patient education is essential: Knowing that telogen effluvium is temporary and that hair usually grows back helps reduce anxiety and makes managing the condition much easier.
Bottom line: Understanding what’s happening with your hair is half the battle—most people see recovery once the trigger is addressed.
Telogen Effluvium Treatment Options: Regrowing Hair Effectively
The best news about Telogen Effluvium (TE) is that it’s nearly always temporary! The main goal of treatment isn’t to start a new drug, but to find and fix the problem that shocked your body, allowing your hair to regrow naturally.
To explore treatment options, the Cleveland Clinic’s hair loss treatment page is a useful resource.
1. The Core Strategy: Stop the Stress, Start the Recovery
Because TE is a reaction to a trigger, the first step is always the most important. You must identify and address the underlying trigger that caused the shock (like a severe illness, crash diet, or major stress). Once the cause is gone, your hair cycle will naturally reset.
- Be Patient: Full regrowth takes time, typically 6 to 12 months after the trigger is removed. The shedding you see is often a sign that the new, healthy hair is already growing underneath!
- Counseling is Key: Understanding this long timeline is essential. Reassurance from a doctor that your hair will grow back helps manage the significant distress caused by the shedding.
2. Fixing Hidden Deficiencies (The Power of Nutrition)
Hair is non-essential, so when your body is low on nutrients, hair follicles are the first to lose resources. Blood tests can confirm if these are your triggers, making correction a direct and powerful intervention:
Iron (Ferritin) Repletion:
Iron is essential for the hair growth cycle. Low iron can cause shedding even if you’re not anemic. For best results, your doctor will aim to maintain serum ferritin levels above 40 ng/dL and optimally 70 ng/dL. To help your body absorb iron better, be sure to take it alongside Vitamin C.
Other Key Vitamins
- Vitamin D: If a deficiency is confirmed by blood work, supplementation is recommended, as low levels are associated with TE.
- A Warning About Vitamin A: Be careful with high-dose supplements! Excessive Vitamin A intake (hypervitaminosis A) is a recognized cause of hair shedding.
- Supplementation Cautions: Supplements like Biotin, zinc, or B12 are not routinely recommended for TE correction, as evidence is lacking. Biotin, in particular, can interfere with crucial blood tests (like thyroid function) and should often be paused during diagnosis.
3. Boosting Regrowth (For Chronic or Slow Cases)
Pharmacological Intervention:
- Topical Minoxidil (e.g., Rogaine): This is the only suggested pharmacological option for Chronic TE. Applied directly to the scalp, it acts as a non-hormonal growth stimulant to shorten the resting phase. Keep in mind that clinical results for TE can be variable.
Advanced and Supportive Therapies
- Platelet-Rich Plasma (PRP) Therapy: This involves concentrating growth factors from your own blood and injecting the solution into the scalp to stimulate dormant follicles to re-enter the growth phase.
- Low-Level Laser Therapy (LLLT): At-home devices (combs, helmets) use gentle laser light to stimulate and energize hair follicles, potentially improving hair density and speeding up recovery.
Preventing Telogen Effluvium: Tips for a Healthy Hair Cycle
Since Telogen Effluvium (TE) is a reactive condition, many episodes are preventable simply by protecting your body from the sudden “shocks” that disrupt the hair cycle. Focus on these proactive strategies to keep your hair healthy and strong:
1. Guard Your Nutritional Reserves
Protecting your hair starts with maintaining stable, adequate resources in your body.
- Avoid Crash Dieting: Aim for gradual, sustainable weight loss rather than rapid, restrictive diets that create a massive caloric or protein deficit. Sudden deprivation signals starvation to your body, forcing resources away from hair growth.
- Ensure Protein Intake: Since hair is made of protein, make sure your daily diet includes consistent, high-quality protein sources (lean meats, fish, eggs, legumes).
- Monitor and Treat Deficiencies: Don’t wait for shedding to start. Ask your doctor for routine blood work to check your iron (ferritin) and Vitamin D levels. Correcting low levels proactively is the best form of prevention.
- Mind Your Vitamin A: Be cautious with high-dose supplements, as excessive Vitamin A intake (hypervitaminosis A) is a recognized cause of hair loss.
2. Build Physical and Emotional Resilience
Emotional and physical stress are the most common triggers for TE. Managing them is essential for prevention.
- Practice Proactive Stress Management: Incorporate daily stress-reduction habits like mindfulness, yoga, deep breathing, or regular exercise to keep stress hormones (like cortisol) from spiking to a critical “shock” level.
- Prioritize Consistent Sleep: Poor or inconsistent sleep is a major physical stressor. Aim for 7–9 hours of quality rest per night to help regulate your body’s restorative processes, including the hair cycle.
- Plan for Major Events: If you know you have major surgery or significant trauma coming up, discuss preventative nutritional and recovery strategies with your medical team in the months leading up to the event.
3. Communicate with Your Healthcare Team
Address potential medical triggers before they affect your hair.
- Manage Underlying Health: Ensure any chronic conditions, such as thyroid disorders or autoimmune diseases, are well-controlled through continuous management and appropriate medication.
- Review New Medications: If a doctor prescribes a new drug, especially one known to occasionally cause hair loss (see the Causes section), ask about alternatives or agree on a monitoring plan with your physician. Never stop a prescribed medication without your doctor’s guidance.
Telogen Effluvium Myths vs Facts: Common Hair Loss Misconceptions
Myth 1: The shedding means I am going bald permanently.
- Fact: TE is a temporary condition. The follicles are not damaged, and full recovery is the expected outcome once the trigger is resolved.
Myth 2: Washing, brushing, or coloring my hair causes the shedding.
- Fact: These activities only release the hairs that were already scheduled to fall out. They do not cause the condition or increase the rate of loss.
Myth 3: Hair falls out immediately after a stressful event.
- Fact: There is a mandatory 2-to-4-month delay. The shedding you see today is a reaction to something that happened weeks or months ago.
Myth 4: The white bulb on the hair is the root, and the hair is dead forever.
- Fact: The white bulb is the non-living club end of a resting hair. Its presence means the follicle is healthy and is already growing a new hair beneath it.
Myth 5: I need a special shampoo or vitamin to stop the shedding.
- Fact: No product can stop the active shedding phase. The only effective treatment is to identify and eliminate the underlying trigger (e.g., correct a deficiency, reduce stress).
Frequently Asked Questions About Telogen Effluvium (TE)
1. What exactly causes this sudden, excessive hair shedding?
TE is triggered by a major physical or emotional stress that shocks the hair cycle. Common causes include a high fever (from illness), severe emotional stress, major surgery, significant crash dieting/weight loss, childbirth (postpartum TE), and certain medications or nutrient deficiencies (like iron/ferritin).
2. Why am I noticing the hair loss now?
There is a characteristic 2-to-4-month delay. The stressful event causes the hair to prematurely enter the resting phase today, but it doesn’t shed until the end of that resting phase, which is 2 to 4 months later. You need to look back at what happened in your life a few months ago.
3. Is my hair loss permanent? Will I go bald?
No. TE is temporary and reversible. It causes diffuse (all-over) thinning, but the hair follicles are still alive and healthy. You will not go completely bald. The hair will grow back once the underlying cause is resolved.
4. How long does the shedding phase last?
Acute TE (most common): The heavy shedding usually lasts between 3 and 6 months after the initial trigger is removed and the body recovers.
Chronic TE: This lasts longer than six months and usually indicates an ongoing, unresolved issue (like a long-term nutritional deficit).
5. What is the white bulb I see on the shed hair?
The small white tip is the keratinized “club” end of a telogen (resting) hair. It is not the living hair root. Its presence actually confirms it is a telogen hair, and it means a new hair is already being formed to push it out.
6. Can I speed up the regrowth or stop the shedding with shampoo/supplements?
You cannot instantly stop the shedding phase, as those hairs are already detached. The best “treatment” is to identify and correct the root cause (e.g., manage stress, correct an iron or vitamin D deficiency). Supplements like Biotin or specific hair vitamins may support growth but will not stop the shedding process itself.
Conclusion: Recovering From Telogen Effluvium and Promoting Hair Regrowth
Telogen Effluvium (TE) is a frightening experience, but the key takeaway is that it is almost always temporary and fully reversible.
The shedding you see is simply a delayed reaction to a stress, illness, or deficiency that occurred 2 to 4 months ago. The most effective course of action is not to use special products, but to:
- Identify and Correct the Root Cause: Get blood tests (especially for iron/ferritin and thyroid) and actively manage stress.
- Be Patient: Once the trigger is addressed, the hair follicles will restart growth. While the shedding phase lasts 3 to 6 months, full density recovery takes time, typically 6 to 18 months.
Focus on healing your body, and your hair will follow.
Related Posts
Learn how male pattern baldness differs from temporary hair shedding like Telogen Effluvium.
See the stages of male pattern baldness to compare with temporary hair loss patterns.