Introduction
For many, Finasteride works as promised — helping with confidence and slowing hair loss. But for a small number of people, the story doesn’t end when they stop the pill.
Weeks or months later, they still feel “off” — dealing with low energy, sexual changes, or brain fog that just won’t go away.
These lingering issues, often called finasteride persistent side effects, have led to what doctors and researchers now refer to as Post-Finasteride Syndrome (PFS).
It’s a rare but distressing condition that can affect both the body and mind. Understanding what PFS is — and why it happens — is the first step toward finding answers and support.

Table of Contents
What Is Post-Finasteride Syndrome (PFS)?
Post-Finasteride Syndrome (PFS) is a condition where certain side effects of Finasteride continue even after stopping the medication.
These lingering effects can involve changes in sexual function, mood, energy, and cognition, lasting weeks, months, or—rarely—years.
It’s believed to occur when Finasteride disrupts key hormonal and neurological balances in the body, leading to symptoms that persist beyond treatment.
While uncommon, PFS can have a significant impact on quality of life and deserves careful medical attention and awareness.
Is Post-Finasteride Syndrome Real?
The question of whether PFS is real has become one of the most discussed topics among Finasteride users. Thousands of men online describe ongoing changes in their body and mind after stopping the medication — while researchers continue to search for solid medical proof.
What Patients Report
Many former Finasteride users say their side effects didn’t go away even after stopping the drug. They describe symptoms such as low libido, fatigue, emotional numbness, and brain fog that last for months or even years.
For them, PFS feels undeniably real — affecting daily life, relationships, and confidence. These shared experiences have pushed doctors and researchers to take a closer look.
What Researchers Say
So far, medical research hasn’t confirmed exactly why some people experience persistent effects. Studies have explored hormonal and neurochemical changes, but there’s still no single test or explanation that proves the cause.
Scientists acknowledge that these symptoms are real for patients and are continuing to investigate how Finasteride might lead to such long-term reactions.
In short: While patient experiences strongly suggest PFS is real, science is still uncovering the biological reasons behind it — which leads us to the next question: what actually causes Post-Finasteride Syndrome?
What Causes Post-Finasteride Syndrome?
Researchers still don’t fully understand why some men experience long-lasting side effects after stopping Finasteride — but it’s believed to be connected to how the drug changes hormone activity and brain chemistry.
Finasteride is commonly prescribed for two main conditions:
- Male pattern hair loss (Androgenetic Alopecia) – usually treated with Finasteride 1 mg, which helps slow thinning and stimulate regrowth.
- Benign Prostatic Hyperplasia (BPH) – typically treated with Finasteride 5 mg, to reduce prostate size and improve urinary symptoms.
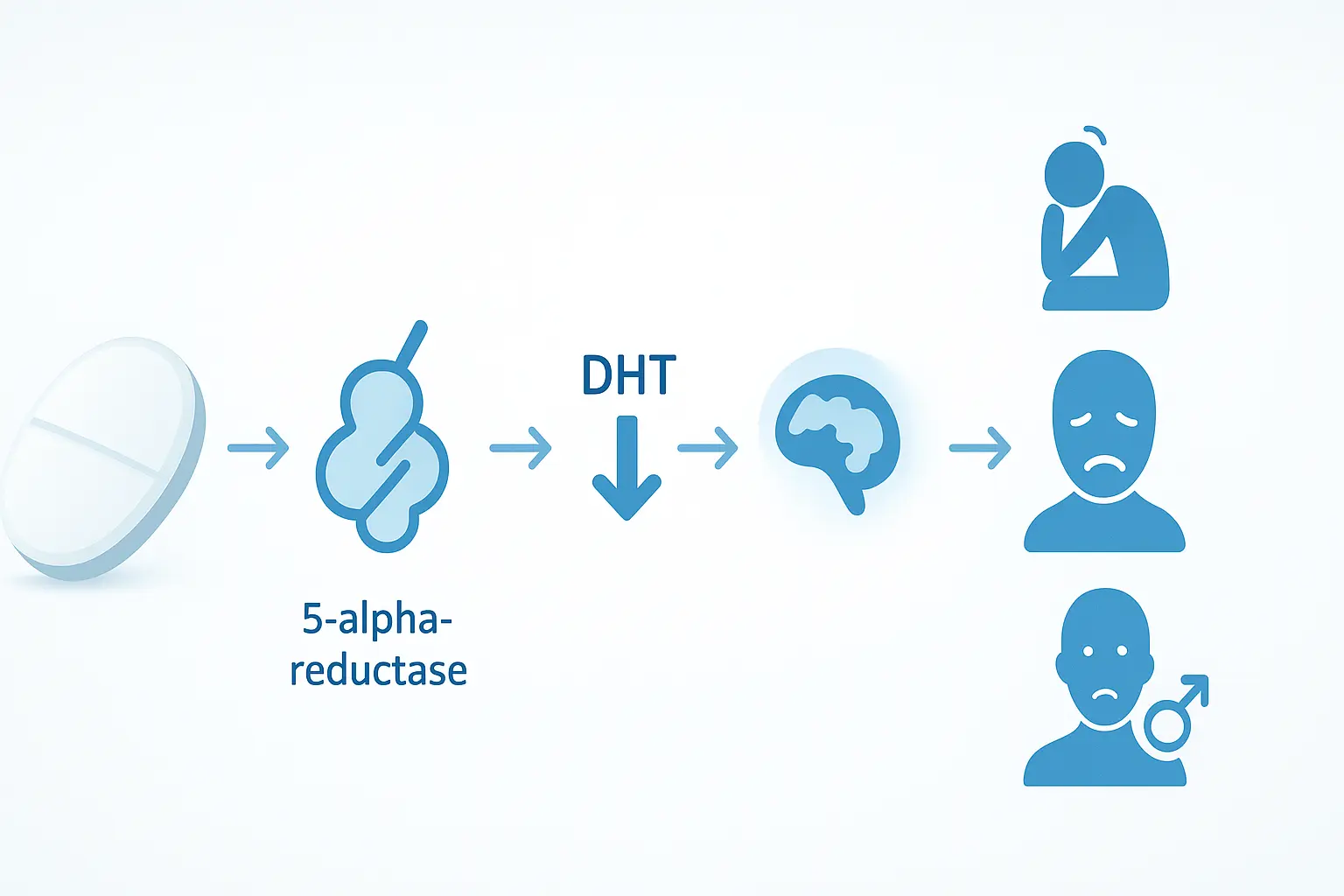
The medication works by blocking the enzyme 5-alpha-reductase, which converts testosterone into DHT (dihydrotestosterone).
While lowering DHT helps in these conditions, it can also disturb other hormonal and neurological pathways that regulate mood, sleep, sexual health, and overall energy.
Some users report that these effects don’t fully disappear after discontinuing the drug — leading to what’s described as Post-Finasteride Syndrome (PFS) or persistent side effects.
Here’s what experts believe could play a role:
- Hormonal imbalance: Lower DHT may disrupt testosterone and estrogen balance.
- Neurosteroid disruption: Finasteride reduces certain brain chemicals (like allopregnanolone) involved in mood and calmness.
- Genetic susceptibility: Some individuals may be more sensitive to DHT changes.
- Metabolism differences: Each body processes Finasteride differently, which might affect recovery speed.
Although ongoing studies haven’t found one clear cause, most experts agree PFS is rare. Still, understanding these possible mechanisms helps users make informed and careful choices when considering Finasteride.
Symptoms of Post-Finasteride Syndrome
Post-Finasteride Syndrome (PFS) occurs when certain side effects of Finasteride don’t go away after stopping the medication. These symptoms can persist for months or even years, affecting sexual, mental, and physical health.
1. Sexual Symptoms
PFS often causes long-term changes in sexual function that continue despite normal hormone levels.
Common symptoms include:
- Ongoing low libido or loss of sexual desire
- Persistent erectile dysfunction
- Absence of morning or spontaneous erections
- Reduced semen volume or dry ejaculation
- Genital numbness or reduced sensitivity
- Shrinkage of penile or scrotal tissue
- Gynecomastia (breast tissue changes)
These persistent symptoms can deeply affect confidence, intimacy, and overall quality of life.
2. Neuropsychiatric & Cognitive Symptoms
Finasteride can alter brain neurosteroid levels, which may affect mood and cognition.
Commonly reported symptoms include:
- Persistent depression or anxiety
- Emotional numbness or loss of pleasure (anhedonia)
- Trouble focusing, memory loss, or brain fog
- Panic attacks and sleep disturbances
A clinical study published in the Journal of Clinical Psychiatry (Irwig MS, 2012) found that:
- 75% of former Finasteride users with persistent sexual side effects experienced depressive symptoms, and
- 44% reported suicidal thoughts, compared to only 3% in the control group.
These findings suggest a potential neurochemical link between Finasteride use and mood changes, though the exact mechanism remains under study.
You can read the full NIH-backed study here:
Depressive symptoms and suicidal thoughts among former users of Finasteride (PubMed)
3. Physical & Systemic Symptoms
In addition to sexual and psychological symptoms, PFS can also cause physical and metabolic effects that may vary in severity.
Reported symptoms include:
- Chronic fatigue or low energy
- Muscle weakness or loss
- Dry skin, reduced sebum, or thinner hair Joint or muscle pain
- Cold sensitivity or reduced body temperature
- Changes in body composition or weight
If these issues persist after stopping Finasteride, consult a healthcare provider for hormone and neurological evaluation.
⚠️ When to Seek Medical Help
If you notice persistent sexual, emotional, or physical symptoms after using or discontinuing Finasteride, consult a doctor, endocrinologist, or psychiatrist. Early evaluation and supportive care can significantly improve your recovery.
Side Effects of Finasteride (During Use)
These are temporary, expected reactions that some men experience while taking Finasteride. They usually resolve after the body adjusts or the medication is stopped.
Common Temporary Side Effects
- Mild loss of libido
- Erectile difficulties
- Reduced semen volume
- Testicular discomfort
- Breast tenderness or swelling
- Dizziness or mild fatigue
Diagnosis: How Is Post-Finasteride Syndrome Diagnosed?
Diagnosing Post-Finasteride Syndrome (PFS) can be challenging because there is no single test that confirms it. Instead, doctors look at your medical history, symptoms, and hormone levels to determine whether the condition fits the PFS pattern.
Since symptoms often overlap with other issues like stress, low testosterone, or thyroid problems, it’s important to get a comprehensive medical evaluation rather than self-diagnosing.
Here’s how doctors usually approach a possible Finasteride syndrome diagnosis:
1. Medical History Review
Your doctor will discuss:
- When you started and stopped Finasteride
- The dosage used (typically 0.5 mg or 1 mg for hair loss)
- When symptoms appeared and how long they’ve lasted
This helps identify whether symptoms began after Finasteride use or have another underlying cause.
2. Symptom Assessment
You may be asked about:
- Sexual function
- Energy, sleep, and fatigue
- Emotional and cognitive changes
3. Hormone & Blood Tests
To rule out other conditions, your doctor may recommend:
- Testosterone and DHT levels (to assess androgen balance)
- LH and FSH hormones (for pituitary function)
- Thyroid function tests
- Vitamin D and B12 levels
These tests help identify if the symptoms are due to hormonal imbalance or nutrient deficiencies instead of PFS.
4. Psychological Evaluation
Because some symptoms involve mood or cognitive changes, doctors may also perform a mental health assessment to check for anxiety, depression, or sleep-related issues that can mimic PFS.
5. Diagnosis of Exclusion
Currently, Post-Finasteride Syndrome is diagnosed by exclusion — meaning other possible causes must be ruled out first. Only after this process can a doctor conclude that the symptoms are consistent with PFS.
Key Takeaway:
If you suspect you may have Post-Finasteride Syndrome, avoid self-diagnosis or panic. Instead, visit a qualified dermatologist, urologist, or endocrinologist who can evaluate your symptoms and perform the right tests.
Early evaluation and lifestyle support can help manage symptoms and improve recovery outcomes.
Recovery and Treatment for Post-Finasteride Syndrome (PFS)
Recovery from PFS can vary widely between individuals. There is currently no specific cure, but many men report gradual improvement with medical support, lifestyle changes, and patience.
Here are some common approaches to PFS recovery:
1. Medical Evaluation and Hormone Testing
A healthcare provider may recommend blood tests to check hormone levels such as testosterone, DHT, estrogen, and cortisol. Balancing these hormones through supervised treatment can sometimes ease symptoms related to Finasteride syndrome.
2. Mental Health Support
PFS can impact mood, energy, and cognitive function. Working with a psychologist or psychiatrist can help manage anxiety, depression, and brain fog. Approaches like Cognitive Behavioral Therapy (CBT), mindfulness, and stress management are often beneficial.
3. Nutrition and Lifestyle Changes
A balanced diet rich in omega-3 fatty acids, zinc, magnesium, and B vitamins may support hormone balance and nerve health. Regular exercise, good sleep, and limiting alcohol or excessive caffeine can also improve overall well-being.
4. Gradual Symptom Management
Doctors may focus on treating individual symptoms, such as:
- Sexual health: Using medications or supplements (only under medical advice).
- Fatigue: Improving sleep patterns and energy through physical activity.
- Mood changes: Supporting mental health with therapy or safe medication.
5. Patience and Support Networks
Recovery can take months to a few years. Joining online support groups or PFS recovery communities can provide guidance, encouragement, and emotional support.

Important: Avoid self-medicating or using unproven “PFS cures” found online. Always consult a qualified doctor or endocrinologist before starting any treatment.
Persistent Side Effects (Post-Finasteride Syndrome)
In a small number of users, some side effects continue even after the drug is stopped, sometimes for months or years.
These long-lasting effects are what define Post-Finasteride Syndrome (PFS).
They may include:
- Ongoing loss of sexual function (libido, arousal, or performance issues)
- Genital numbness or reduced sensitivity
- Depression, anxiety, or emotional flatness
- Sleep disturbances and brain fog
- Muscle loss or fatigue
- Persistent changes in body composition or energy levels
Most users find these effects improve within a few weeks to months of stopping the medication.
⚠️ When to Seek Medical Help:
If you notice sexual, neurological, or emotional symptoms that do not improve after stopping Finasteride, it’s important to discuss them with a qualified healthcare provider.
While the exact cause of PFS is still being researched, early recognition and support can help manage symptoms more effectively.
Can Post-Finasteride Syndrome (PFS) Be Prevented?
While Post-Finasteride Syndrome (PFS) is rare, it’s understandable to want to minimize the risk. The best prevention is responsible and monitored use of Finasteride under medical supervision.
Here are some tips that may help reduce the chances of developing Finasteride syndrome:
- Start with the lowest effective dose: Some doctors recommend beginning with 0.5 mg or even lower doses before increasing gradually.
- Regular follow-ups: Schedule routine hormone check-ups if you’re taking Finasteride long term. Avoid abrupt discontinuation: Stopping the medication suddenly may increase the risk of temporary hormonal imbalance.
- Report side effects early: If you experience unusual fatigue, mood changes, or sexual issues, talk to your doctor immediately.
- Maintain a healthy lifestyle: Balanced diet, stress control, and good sleep can support hormone stability.
Remember, most Finasteride users never develop PFS — but being cautious, informed, and proactive can make a big difference.
When to See a Doctor
If you notice persistent symptoms such as low libido, depression, or fatigue after stopping Finasteride, it’s important to consult a healthcare professional or endocrinologist. They can evaluate your hormone levels, guide treatment, and help monitor your recovery safely.
Getting timely support not only improves your chances of recovery but also helps prevent symptoms from worsening over time.
FAQs — Post-Finasteride Syndrome
What is Post-Finasteride Syndrome (PFS)?
Post-Finasteride Syndrome (PFS) describes a set of persistent symptoms — sexual, neuropsychiatric, and physical — that occur in some men after stopping Finasteride. Symptoms can last weeks, months, or longer in rare cases.
Can PFS happen if I never took Finasteride?
No. By definition PFS only occurs in people who have taken Finasteride (or a similar 5α-reductase inhibitor like Dutasteride). Similar symptoms can result from other conditions, but those are not PFS.
Can low doses (0.5–1 mg) of Finasteride cause PFS?
Yes — although rare, cases of persistent symptoms have been reported at typical hair-loss doses (0.5–1 mg). Most users do not develop PFS.
What are the common symptoms of PFS?
Symptoms commonly fall into three groups: sexual (low libido, erectile dysfunction, reduced semen volume, genital numbness), neuropsychiatric (depression, anxiety, brain fog, memory problems), and physical (fatigue, muscle weakness, dry skin, metabolic changes).
Is Post Finasteride Syndrome permanent?
Not necessarily. Many people improve over time after stopping Finasteride; some recover fully while others have longer courses. A small number report symptoms that persist long term. Research is ongoing.
Should I stop Finasteride if I have side effects?
If you experience troubling side effects, speak with your prescribing doctor before stopping. If you experience severe mood changes or suicidal thoughts, seek immediate medical help — do not delay.
Conclusion
Post-Finasteride Syndrome (PFS) remains a complex and often misunderstood condition affecting some individuals even after stopping Finasteride. Its symptoms—ranging from sexual dysfunction to mood and cognitive changes—can significantly impact quality of life.
While research on PFS is ongoing, current evidence highlights the importance of early awareness, medical supervision, and mental health support for those experiencing persistent side effects. Anyone noticing long-term symptoms after discontinuing Finasteride should consult a qualified healthcare professional for evaluation and guidance.
Ultimately, understanding PFS encourages informed decision-making about Finasteride use and promotes open discussion between patients and doctors about potential risks and benefits.
⚠️ Medical Disclaimer
This article is for educational and informational purposes only. It does not replace professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare provider before making decisions about medications or managing health symptoms.
Related Posts
Learn how Finasteride works, its benefits, and safety tips.
Discover the causes of hair loss and explore effective treatments for thinning hair.
See how Minoxidil can help slow hair loss and promote regrowth.
Understand the stages of male pattern baldness and how hair loss progresses.